A Brief History of Deductibles
Deductibles have been around since the 1940s... people hated cost sharing back then too
Waiting Room is a blog that explains incentive misalignments in healthcare and health tech. Today, we’re covering deductibles.
High deductible health plans (HDHPs) are the most common plans on public ACA exchanges and chosen by 50% of policyholders who receive insurance from their employer. Named after the signature cost sharing mechanism, the (high) deductible is a set dollar amount that a consumer must spend on care before their health insurance actually kicks in. The annual deductible for an individual averages $2,000 and $4,000 for a family (maxing out in some states at a whopping $6K and $12K, respectively).
Insurers claim that deductibles bring down expenses by forcing consumers to make better health and wellness choices. But deductibles create perverse consequences. Few Americans (14%) fully understand the deductible alongside monthly premiums and don’t evaluate it when picking insurance. 64% of consumers on HDHPs avoid seeking care at all, knowing they’ll be on the hook for thousands of dollars.
If deductibles are so confusing and even harm consumers, where did they come from? How did they become a fixed feature in healthcare?
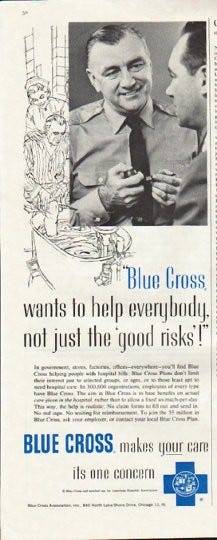
The story starts with hospitals, who made the first venture into health insurance in 1938. Under severe financial strain during the Great Depression, hospitals banded together and created the Blue Cross plans for labor unions. Workers paid monthly premiums to hospitals in additional to normal union dues; they didn’t pay anything out of their own pockets if taken and treated at a hospital until a certain threshold was crossed. The Blue Cross plans proved immensely popular… for a time.
By the 1950s, the limitations were apparent: care for chronic and catastrophic illnesses, alongside rising medical costs, made Blue Cross plans less financially viable for hospitals. Policyholders (primarily labor union members) also sought coverage outside of hospitals like primary care and dental.
Private companies stepped in with a new kind of insurance called “major medical.”

(I WISH this was Major Medical but The General sadly just sells auto insurance with Shaq??)
Major medical covered hospital expenses as well as diagnostic testing, outpatient procedures, and preventative primary care visits. To provide more coverage for less than the cost of a Blue Cross plan, major medical insurance required a deductible and coinsurance/copayments, the standard amount or percentage paid each time a covered service was used.
In simple terms: where Blue Cross had a ceiling, major medical had a floor.
(Now for a quick aside on the economics of deductibles. Deductibles intend to lower premiums and prevent abuse and overuse by policyholders. Since insurance plans with deductibles do not pay the full cost of care, deductibles reduce the amount insurance companies pay overall. Presumably the savings are passed on to the purchaser in the form of lower premiums. On the subject of abuse and overuse, the central principle of insurance is protection against unanticipated risk. Insurers don’t want - and don’t permit - people to sign up for coverage only when they are sick because it abuses that principle. Deductibles are also a way to discourage overutilization of health services, derisively called “sniffle claims.”)
Employers celebrated deductibles on ideological grounds, particularly at a time when workers demanded more benefits. In the words of executive Charles Hayden in 1953, if the worker "has to pay for it out of his own pocket, it becomes a matter of, ‘how can I best spend this money and get the most out of it?’ If he is spending somebody else's money, he does not give a damn.” Deductibles and other forms of cost sharing were reminders that health insurance was a purchasable product, not an entitlement to free care. Even the American Medical Association supported cost sharing, believing deductibles and copays supported physician autonomy and prevented overwork.
Major medical insurance, with its signature deductible, was adopted rapidly. Between 1951 and 1961, the number of people covered by major medical through employers increased from 108,000 to 34 million.

But healthcare outcomes in the 1960s began showing the negative effects of deductibles and copays. The AFL-CIO countered that deductibles worked against union demands for improved access to healthcare. This lead the RAND Institute to conduct a series called the “Health Insurance Experiments,” placing thousands of families on 15 insurance plans. RAND concluded that deductibles increased cost and care barriers particularly for low income people and large families. Both of these groups spend more on care (due to chronic conditions for the low income and regular pediatric visits for families), and are more likely to face bankruptcy than other populations.
Brookings Institute health analysts Anne and Herman Somers wrote in 1961 that there remained a “discrepancy between hope and fulfillment in major medical benefit coverage.” It still excluded many services like maternity care. The Somerses also argued that major medical drove up the price of health care. By placing initial cost containment on consumers (and not providers) through deductibles and covering catastrophic hospital bills, major medical de-prioritized preventative care and encouraged hospitals to set higher fees.
We haven’t talked much about Medicare but it, too, incorporated deductibles from its 1965 inception.
The deductible foreshadowed political debates that continue after the Affordable Care Act. Patients paid 8% of their medical costs in 2007 but pay closer to 33% today. HDHPs offer little protection from the 530,000 medical bankruptcies each year. With deductibles still climbing, people seek alternatives in telehealth and cash pay for procedures like a CAT scan because these options are often cheaper than using insurance. Insurers typically cover one annual visit for free but it’s not benevolent coverage. Blue Cross, Aetna, United… they want to map medical conditions in their population to mitigate and manage risk.

NBC had a segment in 1972 called, "What good is health insurance if it doesn't cover your needs?" Policyholders are still at a disadvantage today, lacking information and optionality. An HDHP is not an inherently bad choice if you have a chronic condition but the average person is not healthcare literate (necessary for choosing the ‘right’ insurance) and few alternatives exist to HDHPs that don’t break the bank.
This brings us to the goal of Waiting Room: highlighting incentive misalignments. In the absence of proper rules that correctly reward or penalize participants, people and organizations act in their own self-interest. It seems like the intention behind deductibles, incentivizing Americans to make better wellness choices, has instead manifested in care avoidance and bankruptcies. Consumers end up weighing the benefits of cost versus care, with care out of reach for many, to the benefit of health systems, insurers, and employers.
Update:
Kevin Wang, of Measure Twice, Cut Once, emailed me about a recent post in Health Affairs on value-based high-deductible plans (VHDP). VHDPs make cost sharing a joint effort between consumers and insurers; insurers incentivize members with exemptions/lower deductibles and copays for choosing specific actions that reduce costs and prioritize preventive care. E.g. higher copays on low-value treatments or brand-name drugs and lower copays on high-value treatments and generic drugs. I love this framework for plan design and hope we see it replace traditional HDHPs.
If you liked this post from Waiting Room, subscribe for more.



