Diagnostic Tattoos and My Sidequest to Become a Heilpraktikerin in Germany
I’m finally back in the States after a few months of purposeful exploration in Berlin. Armed with speculations on the future of healthcare and bio, my next post will be observations for 2022. A quick taste: molecular APIs, remote therapeutic monitoring (RTM), Retool/internal tools for healthcare companies, epigenetic clocks, chemputation, and ascendancy of healthcare influencers.
Wishing you a restful end of the year! I hope 2022 brings a more rebellious streak to healthcare.
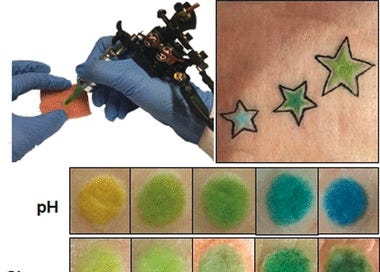
Biosensing Tattoos and Stickers
I blame Katie and Sean and Justin for going under the pen numerous times in 2021. I think of the plasma oozing underneath Justin’s clear adhesive bandages; I’ve romanticized Katie’s ox and the black lines of the ouroboros that snakes across Sean’s shoulder.
That’s how I found myself outside a tattoo parlor in Berlin with my face pressed against frigid glass.
I flirted with tattoo ideas in the summer but my renewed interest comes from a growing body of research on diagnostic biosensors.
At Munich’s Technische Universitüt and Harvard, teams under Virj Kan and Ali Yetisen have developed nanoparticle biochemical sensors. These biosensors function as permanent colorimetric pigments. Instead of tattoo ink, researchers injected the pigments into the thin dermis layer of tissue that hosts nerves, blood vessels, and interstitial fluid (ISF). Sensors vary in color as they come into contact with biomolecules.
Placed appropriately, a diagnostic tattoo can reveal biomarker changes faster than conventional testing and the appearance of symptoms.
Disposable CGMs are amongst the few consumer wearables capable of monitoring at a molecular level (GraphWear and biolinq are attempting needleless glucose monitoring via sweat). Whoop and Oura employ infrared sensors to evaluate hemoglobin levels in blood oxygen. Nanoparticle-based diagnostic tattoos expand detection further and are able to monitor organic molecules, proteins, DNA, bacteria/viruses, and even drugs. Carbon and gold nanoparticles are common catalysts - exhibiting color changes distinguishable to the naked eye.
Yetisen has experimented with microfluidic point-of-care devices for almost a decade. He’s built a contact lens with ocular diagnostic capabilities, and his work serves as inspiration for companies like LogicInk that develop biochemical-sensing stickers.
Consumer health is a strange commingling of desirability and mortality, where man and his technological marvels coexist in uneasy equilibrium. We now design wearables and devices for conspicuous consumption. But the quantified self is still a kind of countdown (hey! at least we looked good heading towards inevitable, final rest).
These are tradeoffs we will always make in healthcare.
Nonetheless, diagnostic tattoos and stickers are credible, less painful alternatives to repetitive blood biopsies. They are also cosmetic displays with clear qualitative readouts, enabling people of all ages and abilities to monitor their functional health.
Healthcare is guilty of paralyzing patients with information overload. Research indicates that throughout the industrialized world, protocols for disease prevention, management, and care have increased in complexity and require sophisticated health literacy skills. If medical information is above an 8th grade reading level, patients are “less likely to engage in preventive activities, participate in screening… or know about their illness.” State Medicaid agencies recommend material written at a 6th grade level. Most health information fails to meet these guidelines.
Diagnostic tattoos and stickers sidestep this issue by symbolizing health information. Perhaps trite but Apple elegantly shows available device storage alongside recommendations. Contrast that with results from a blood test:
Dynamic visuals don’t have to infantilize. Biosensing tattoos and stickers offer a concise, creative ways to communicate health information in real-time. And, perhaps, they get us a closer to the visionary future of medical care we were promised.
Bist du eine heilpraktikerin?
I often showed up to Mano, a Kreuzberg cafe, with a dog-eared book, espresso craving, and the appetite to chat with a stranger:
On an odd Wednesday, I’m at Mano with a proteomics postdoc named Till and his physician friends from Charité. We’re two glühweins in and discussing the differences between German and American healthcare (particularly, the American posture towards experimental treatments).
“So you’re not a doctor or nurse… have you considered becoming a heilpraktikerin?” one of them asks.
He explains the dark origins of the heilpraktiker (HP). The formal profession emerged as a Third Reich provision to expand the medical force and incorporate Germany’s naturopathic undercurrent into an established field. It would not be unreasonable to compare HPs to the U.S. Army’s deployable medical corp. After WW2, the medical establishment split into medical GPs and complementary alternative medical (CAM) practitioners.
Partially covered by private insurance for CAM, heilpraktikers can administer acupuncture, phytotherapy (plant-based medicine), nutritional therapy, kinesiology (physical therapy), and behavioral therapy. HPs can run blood glucose a1c tests and ultrasounds amongst their diagnostic tool kits. They have fixed prescribing privileges. Nearly half of all medical schools in Germany offer HP specializations, and like other clinicians, heilpraktikers must refer to a specialist when they reach the limits of knowledge and available treatments.
Beyond a secondary degree and > 25-year-old age requirement, there are no formal training requisites. HPs need only sit one exam administered by regional health authorities. That doesn’t mean it’s easy. 60-90% of examinees fail the Heilpraktikerprüfung.
“Theoretically, you could become a therapist in a few months.”
I joke to Till and his friends that if I did, I could play a small role in ameliorating America’s shortage of mental health professionals. I look up HP exam test prep when I arrive home. It’s a lengthy, curious mix of anatomy, medicine, and law.
The study guide includes questions about respiratory, musculoskeletal, immune, nervous and endocrine systems. I think back to CPR techniques learned in Girl Scouts and read over laborious sections on incubation periods for viruses and infectious diseases. The guide outlines distinctions between adult and adolescent care.
The exam material interplays with the interesting role that HPs assume come July 1st. Next year, Germany’s new e-prescribing law requires all medical practitioners including HPs to adopt digital health infrastructure from Gematik and the Federal Ministry of Health. After an in-person or video consultation, patients will be able to receive a prescription via QR code. Per the act: “doctors or health insurers are required to refrain from assigning prescriptions to specific pharmacies or influence the insured to redeem prescriptions in a specific pharmacy.” At last, an e-Rezept (like American e-prescriptions).
Roughly 50% of Germans saw an HP yearly in the 2000s. With e-prescribing expansion and Germany’s first-mover track record, I foresee a flurry of digital health activity in Europe and HPs playing an outsize role in that care delivery.
If I head back to Berlin, I’ll take the Heilpraktikerprüfung come spring time. Cue the Quizlet flashcards.
Interesting Links and Tweets
The Build Back Better Act is set to pass in 2022, expanding ACA subsidies. Kaiser and others estimate 3-4M+ individuals who qualify for Medicaid will instead sign up for commercial insurance plans on state exchanges. A boon for players like Oscar and Bright Health
An age of new scientific institutes! Congratulations to Patrick Hsu and co. on the launch of Arc:

A new initiative from the Center of Healthcare Strategies and Arnold Ventures to help states meaningfully improve Medicare-Medicaid integration for dual-eligible individuals
While everyone was focused on Covid, Moderna started an internal division called Moderna Genomics (mGx). mGx brings Moderna’s innovations in manufacturing consistent lipid nanoparticles (LNP) to in vivo gene editing. My next blog post on 2022 observations will cover LNPs amongst other methods of novel drug delivery
A survey of interesting health policy papers from 2021:


Hummingbird Ventures’ Shelby Newsad lists 120+ translational labs that have started or are likely to start companies
Thread from Obvious Ventures’ Meera Clark on healthcare trends she’s paying attention to:

Another great essay by Elliot Hershberg on the genetics of immunity
Why do antibiotics exist?, a paper that analogizes antibacterial resistant genes (ARG) as a secret society hazing microbes with “rituals”
MBAs are good for healthcare management, apparently:



Emulate and Ingber preprint shows the cost-effectiveness of organ chip in clinical research (a method for testing that simulates the mechanics and physiological responses of an entire organ). They suggest liver-chips could generate $3 billion annually, and even more in increased R&D productivity
An alarming but important thread illuminating the ways hospitals surveil patients: