Why Anesthesiologists Are Huge Political Donors, "API" for the Body and More
Welcome back. It feels surreal to be writing this dispatch from Berlin, home of the Robert Koch Institute (where the eponymous doctor / Nobel Prize-winning researcher first determined the connection between infectious agents and disease).
HLTH was this week. I missed out (but did make an appearance on a16z’s Clubhouse session with Nikhil and Chris Hogg)! Were there any notable disagreements and fisticuffs? I find these conferences regurgitate the same tired talking points, though they’re definitely good for BD and mingling at happy hours.
Visiting medical and pharmacology history museums is my favorite underappreciated travel activity. I’ve browsed several over the years including Harvard’s Warren Anatomical Museum, University of Basel’s Pharmaziemuseum, and the Medical Museion in Copenhagen. Kei, a friend and interminable researcher/tinkerer for Gnosis, tipped me off to the Wellcome Collection.
Seeking related exhibit recommendations while I’m here 🤲
My (Conspiracy) Theory on the Lobbying Patterns of Anesthesiologists
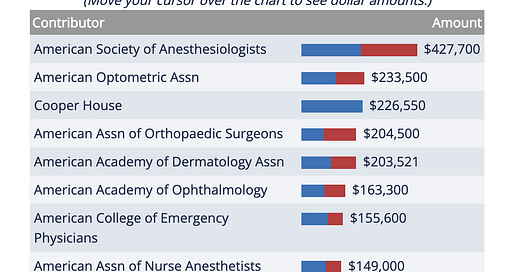
Health professional associations donate… a lot. For a sense of scale, in the 2016 election cycle they gave more than three times the amount contributed by commercial banks. The top 5 groups remain the same year after year: anesthesiologists, ophthalmologists, orthopedic surgeons, dermatologists, and dentists.
All of these specialties are fee-for-service driven, healthy on gross margins, and unsurprisingly private equity darlings / favored roll-up plays.
Contrary to popular belief, anesthesiologists don’t have high rates of malpractice lawsuits (or exorbitant insurance liability); neurosurgeons and OB/GYNs top the list. Tort reform and the pulse oximeter decreased the specialty’s medical malpractice costs by 44% since the ‘80s.
So, let’s hypothesize reasons for all this lobbying:
High salaries and reimbursement - most surgeries (outpatient and hospital inpatient) involve perioperative care. Anesthesiology tends to charge per Time Units (i.e. 60 units is equal to one hour). I’ve never come across episodic or bundled anesthesiology rates for a surgery, which in other specialties promotes lower costs for the same quality care.
Increasingly out of network - anesthesiology service providers are a common source of surprise out-of-network bills (an American Society of Anesthesiologists (ASA) survey claims insurers terminated contracts with 42% of respondents in 2020). While these terminations intend to narrow the network and lower payments, it relegates anesthesiologists into the out-of-network liminal space. Lobbying could protect from further OON changes.
AI conspiracy? - Now I’m really speculating here, but why don’t we have more AI in anesthesiology? It’s one of the few specialties with repeatable parameters and highly reliable inputs → cyclical interpretation and response. Bizarrely, there’s a limited track record of NIH and HHS government funding. Associations are also responsible for promoting research; I could not find much outside of patient safety grants by way of the Anesthesia Patient Safety Foundation. Two studies I found from 2021 say something to the effect of “as more data are being collected, a valid foundation for refinement to the ML will emerge.” We’ve seen radiologists go through this before. Countless studies demonstrate that ML and AI are better than radiologists alone: this recent list of AI/ML FDA-cleared devices is dominated by the radiology category.
Part of me believes this is fear-driven lobbying - AI wouldn’t entirely disintermediate anesthesiologists, and rather complement the role. Perioperative patients sometimes need intubation, for example. I’m happy to be proven wrong if provided convincing evidence to the contrary!
I also encourage someone to build a startup in this space. Value-based care and payments reform will come for anesthesiology, too.
FDA-Cleared vs FDA-Approved Devices
Speaking of the FDA, I recently hung out with HumanFirst CEO and former FDA official Andy Coravos at the co-living community, Radish Oakland. She alerted me to a critical but obscured distinction between FDA-cleared and FDA-approved.
FDA-cleared - the common path for non-invasive and low-risk devices, manufacturers can request a De Novo (new and novel) or 510(k) (mapping to a predictate/substantially similar device) classification. “FDA-cleared” mostly applies to Class I and Class II devices, ranging from bandaids and electric toothbrushes to digital therapeutics, surgical gloves, contact lenses, and pregnancy tests.
FDA-approved - these devices need to prove safety and efficacy through clinical evidence. The pre-market approval (PMA) application is rigorous and can take years but the best assurance of insurance reimbursement. Approved devices include breast implants and deep brain stimulators.
One company that blurs this line to the public is Apple. To much fanfare in 2018, Apple announced that their FDA-cleared Apple Watch contained a proprietary algorithm indicating arrhythmia (related to a heart condition called A-fib). Except the De Novo notification didn’t mean that the Apple Watch’s detection = diagnosis. Clinicians wouldn’t recognize the result and neither would insurance given high false-positivity (34% accuracy in some studies).
In 2020, Apple secured a 510(k) for its new atrial fibrillation classification. Andy pointed out that the updated clearance language maintains the Watch’s results are “[f]or informational purposes only” and “not intended to take a clinical action.” Cleveland Clinic reasonably suggests that “further technological advances are necessary before these wearables can be fully incorporated into current clinical management.”
Total mindfuck but knowing the difference gives you at least a modicum of consumer power.
Nervous System as an Alternative Pathway for Brain Computing?
At least that’s the thesis of Max Hodak, who helped start Neuralink. In his blog, he writes of the promise and limitations in neural engineering. I agree with Max that BCI, for better or for worse, assumes primacy of the cranial nerves.
But the brain isn’t an isolated organ. It’s reacting to a lived environment: the hypothalamus detects biological and emotional stress, the cerebellum initiates motor movement, etc. The central nervous system acts as the major information-processing center, imparting sensory information from the body through the spinal cord to the brain:
These form the complete “API” of the body… The future isn’t better smartphones or AR glasses: it’s making the sensorium itself directly programmable, and maybe even adding new senses entirely.
I’m intrigued. If Max’s new company Science is successful in developing this API, it could herald a step function change towards the full promise of cyborgology and the body as an interface.
Revamping Medical School
Every few months I am seduced into considering medical school. Then I remember the plight of several close friends studying to be an M.D. and quickly return to prognosticating on Twitter.
Tanner Greer, the essayist and researcher behind Scholar Stage, sent me a study on the American residency system which has mutated into a kind of final boss against med students. Up until the 80s, hospitals competed for graduates:
When The Match was first established, there were only 5,800 medical graduates available to fill roughly 10,500 positions.
Then came the implementation of increasingly stringent program requirements combined with tightening public funding, once abundant from Medicare and the G.I. bill. The surplus switched to scarcity. As Charles Evarts, president of the American Orthopaedic Association and a Residency Review Committee member, put it in 1985:
Manpower control is mandatory. The size of medical schools must be diminished; there must be a strict limit upon foreign medical school graduates. Certain programs need to reduce their numbers, others must consolidate, and others need to terminate voluntarily or be terminated… the impending decrease in funding for graduate medical education will directly influence the numbers. Before our destiny is controlled for us, we must step into the breach and exercise considerable leadership.
There was a period in the 1990s when certain specialty physician groups (given scarcity) retained enough market power to reject insurer contracts they deemed unattractive. A reaction to these increased costs and labor shortage emerged in the form of more administrators, nurses, and technicians:
Resident training has become a net cost to hospitals. It’s one instance of a hierarchal and dated medical education in need of modernization. I collected some possible solutions from my friends and docs-in-training Sherman Leung and Morgan Cheatham:
Innovate around admissions by decreasing the influence of the 1910 “Flexner Report.” It’s largely why medical schools still require biochemistry and other non-clinical topics in pre-clinical (and pre-medical) coursework.
Better education around social determinants and health systems thinking.
Hasten the trend of accelerated pathways from school to residency, independent study, and industry work. Some schools have already moved to a 1.5-year pre-clinical timeframe for coursework.
Alternative exposure to clinical medicine without practicing. Stanford’s Masters of Science in Medicine is an example geared towards PhDs. Shadowing a small clinical team (e.g. Medical Assistant-like work) could bridge clinical medicine and industry. Possible tracks for operators interested in pharma/biotech, digital health, etc.
We could also tear it all to the ground and build a hospital - med school from scratch (or buy one and gut it). New tech, advanced clinical protocols, flat leadership/hierarchy.
CMS’s announced strategic directives advance equity and affordability, and there’s no reason medical education reform should be excluded from that. If anyone is reimagining a new kind of med school and/or educational pathway, shoot me an email! I’d love to chat.
Interesting Tweets and Links
Streetwear brand Madhappy, which also runs The Local Optimist (a resource for mental health including interviews, hotlines, etc.), partners with Penn’s Positive Psychology Center:
Propeller founder Chris Hogg announced his new company, Marley Medical, focused on virtual-first chronic care management
Facebook is no longer hiding its biomedical ambitions:
 Re: new Facebook name: “The web address meta.com currently redirects to meta.org, the home of a biomedical research discovery tool developed under the stewardship of the Chan Zuckerberg Initiative.” 👀 bloomberg.com/news/articles/…
Re: new Facebook name: “The web address meta.com currently redirects to meta.org, the home of a biomedical research discovery tool developed under the stewardship of the Chan Zuckerberg Initiative.” 👀 bloomberg.com/news/articles/…New study suggests hygromycin (a known but underutilized compound since the 50s) might be a good candidate for Lyme disease clinical studies
I’m often beating the drum on new research and innovation models (i.e. applied/advanced research projects agencies (ARPAs), @newscienceorg, @vita_dao, @atoms_org). Focused research organizations are having their moment too. Congratulations, Adam and Anastasia!
Another great post from Ed Manzi on fraud and abuse in DME
That one time GlaxoSmithKline went a bit too far with their antidepressant marketing…
The Medicare Advantage STARS program is increasing the weight of customer experience in health plan scores. Notable for any startup selling to insurers
PhD student Gustave Ronteix on why vaccines don’t often drive virus mutations:


---
Thank you to Michael Scognamiglio for thoughtfully reviewing this post and Andy Coravos for her corrections.
Disclosure: The section on FDA-cleared vs. FDA-approved was updated to include the distinction between De Novo and 510(k). I don’t have a copywriter so yolo on the typos. Waiting Room does not represent the views of my employer. I am a scout for a16z’s healthcare and bio team.